Urinary incontinence, which is more common in women after menopause, is the inability to control urination. A significant health problem, urinary incontinence negatively impacts both women's social lives and hygiene.
What causes urinary incontinence in women?
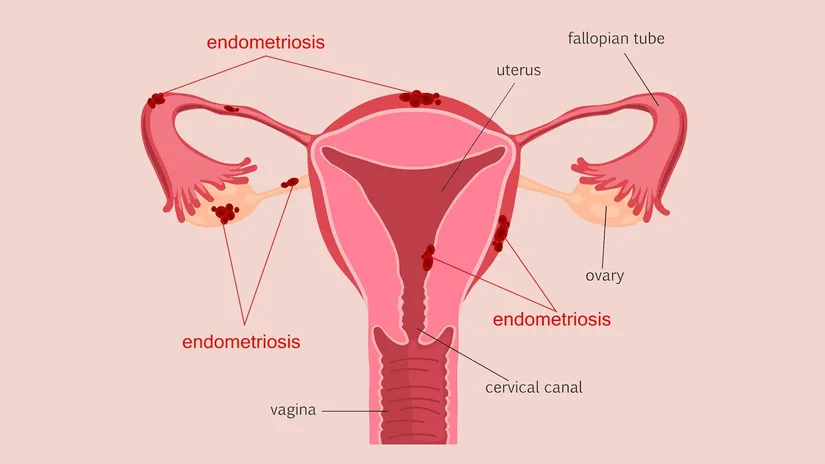
Menopoz öncesi kadınların yaklaşık % 10 ila %30’unu, menopoz sonrası kadınların ise % 35 ila % 56’sını Urinary incontinence, which affects the genital organs, can be observed in conjunction with genital organ prolapse. One of the most important causes of urinary incontinence is genetic predisposition. It can also occur in women who have had difficult deliveries, those who have undergone vaginal surgery in the past, and those with chronic respiratory illnesses. Menopause, radiation therapy, prostate enlargement, urinary tract infections, hormone deficiency, weakness of the pelvic floor muscles, and chronic constipation are also among the factors that cause urinary incontinence.
Types of Urinary Incontinence
There are three types of urinary incontinence. These types vary depending on when and how the patient experiences urinary incontinence.
1. Stress Incontinence (SUI): It occurs as a result of activities that increase intra-abdominal pressure, such as coughing, sneezing, laughing, running and jumping, and lifting heavy loads.
2. Urge Incontinence (UUI): It occurs when the bladder contracts, sometimes without a specific reason, and sometimes as a result of factors such as the sound of water or laughter.
3. Overflow Incontinence: It occurs as a result of the bladder's inability to contract and empty properly, due to various neurological disorders and conditions such as diabetes.
Diagnosis and Treatment of Urinary Incontinence
A thorough history and physical examination are necessary to diagnose the type of urinary incontinence. Additionally, the patient's medical history, bladder diary, urine tests, post-void residual urine measurement, and pad tests are also essential for diagnosis. Treatment for urinary incontinence primarily involves non-surgical methods. These include Kegel exercises (strengthening exercises for the muscles around the vagina), vaginal pessaries (devices to prevent prolapse), electrical stimulation therapies (FESS), and medication. If the patient does not respond to these treatments, or if stress incontinence is present, surgical methods such as sling placement, Burch colposuspension, artificial compression devices (balloon placement), and artificial urinary sphincter (AUS) may be considered.